Veterans
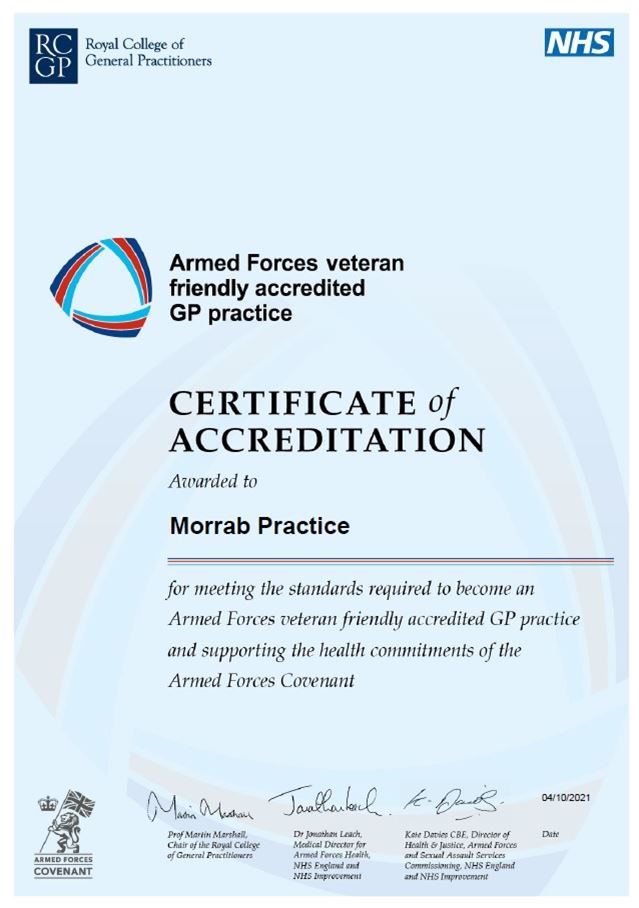
We are delighted to announce that we have now been given Veteran Friendly Practice Status by the Royal College of General Practitioners.
This means that, as part of the health commitments of the Armed Forces Covenant, we have a dedicated clinician who has a specialist knowledge of military related health conditions and veteran specific health services. This is important in helping ex-forces to get the best care and treatment. If you are ex-forces, please let your GP know to help ensure you are getting the best possible care.
What is a veteran?
A veteran is anyone who has served for at least one day in the Armed Forces, whether regular or reserve. It means the same as ‘ex service personnel’ or ‘ex-forces’, although not all veterans know, choose or want to associate with the term ‘veteran’. This is particularly the case amongst younger veterans who often refer to themselves as ‘ex-forces’, due to the common belief that a veteran is someone who fought in the First / Second World War.
What is the Armed Forces Covenant?
The NHS has a duty to deliver on a number of health commitments, which are set out in the Armed Forces Covenant as follows:
- The Armed Forces community should enjoy the same standard of, and access to healthcare as that received by any other UK citizen in the area they live.
- Family members should retain their place on any NHS waiting list, if moved around the UK due to the service person being posted.
- Veterans should receive priority treatment for a condition which relates to their service, subject to clinical need.
- Those injured in service should be cared for in a way that reflects the nation’s moral obligation to them, by healthcare professionals who have an understanding of the Armed Forces culture
This is reflected in principle four of the NHS Constitution, which states ‘the NHS will ensure that in line with the Armed Forces Covenant, those in the Armed Forces, reservists, their families and veterans are not disadvantaged in accessing health services in the area they reside’.
The Covenant is an important aspect of our approach to care, especially as the Armed Forces community can be at a disadvantage due to their mobility and frequent moves.
What dedicated NHS services and support are available to veterans?
Op COURAGE: The Veterans Mental Health and Wellbeing Service, including a new and urgent emergency mental health service for veterans
The NHS has launched Op COURAGE: The Veterans Mental Health and Wellbeing Service, the new overarching name for the three NHS veterans mental health services (Veteran’s Mental Health Transition, Intervention and Liaison Service (TILS), Veteran’s Mental Health Complex Treatment Service (CTS) and Veteran’s Mental Health High Intensity Service (HIS). The new name has been developed by veterans and their families and is intended to make the services easier to find and access.
Veterans’ Mental Health, Transition, Intervention and Liaison Service (TILS)
The TILS is for both serving personnel approaching discharge from the Armed Forces and veterans with mental health difficulties. The service provides a range of treatment, from recognising the early signs of mental health problems and providing access to early support, to therapeutic treatment for complex mental health difficulties and psychological trauma. Help may also be provided with housing, employment, alcohol misuse and social support.
The service comprises three elements:
- Transition: service for those in transition from the Armed Forces
For those due to leave the Armed Forces, the TILS will work with the Ministry of Defence (MOD) to offer individuals mental health support through their transition period and beyond. - Intervention: service for veterans with complex presentation
Service personnel approaching discharge and veterans will have an assessment within two weeks of a receipt of referral. If their needs are identified as suitable for treatment within the TILS, the service will aim to see them for their first appointment two weeks after this. They will be supported by a military aware team who will develop a personalised care plan with the individual. - Liaison: general service for veterans
Patients who do not have complex presentations, yet would benefit from NHS care, will be referred into local mainstream NHS mental health services where they will receive treatment and support. This could include talking therapies or treatment for other conditions, such as eating disorders or psychosis.
Veterans’ Mental Health Complex Treatment Service (CTS)
The CTS is for ex-forces who have military related complex mental health difficulties that have not improved with previous treatment. The service provides intensive care and treatment that may include (but is not limited to) support for drug and alcohol misuse, physical health, employment, housing, relationships and finances, as well as occupational and trauma focused therapies.
Veterans can self-refer or be referred by their GP, a charity or family or friends to access specialist care through this single route Op Courage.
Further details are available on the NHS website.
Contact details are as follow:
- North of England, call 0303 123 1145 or email vwals@nhs.net
- Midlands or East of England, call 0300 323 0137 or email mevs.mhm@nhs.net
- London or South East England, call 020 3317 6818 or email
cim-tr.veteranstilservice-lse@nhs.net - South West of England, call 0300 365 2000 or email gateway@berkshire.nhs.uk
Veterans Trauma Network (VTN)
The VTN is the first NHS pathway for veterans’ physical health, providing care and treatment to those with a service-attributable physical healthcare problem. Located in 13 major trauma centres (Plymouth, Oxford, London (three centres), Birmingham, Nottingham, Liverpool, Leeds and Middlesbrough) across England, the VTN works closely with Defence Medical Services, national centres of clinical expertise, Op COURAGE, as well as military charities to provide a complete package of care. It is run largely by healthcare professionals who are either veterans or serving members of the Armed Forces. GPs can use a single national email to refer veterans to the service (england.veteranstraumanetwork@nhs.net), where they will benefit from specialist care by military and civilian experts.
Prosthetics
The Veterans’ Prosthetics Panel (VPP) was established in 2012 as a way of ensuring that veterans can access high quality prosthetics regardless of which Disablement Service Centre (DSC) they attend. This additional funding is available only to veterans who have lost a limb whilst in military service. A veteran who has left the Armed Forces, but whose limb loss is attributable to an injury sustained whilst in service, also qualifies. Veterans who lose limbs after they leave the military or suffer limb loss whilst in the military, but not in a service attributable incident, such as in a civilian road traffic accident, will continue to access services as usual through their local DSC.
The additional funding for veterans is for treatment that would not typically be provided by the NHS, for example higher specification prostheses than are normally available on the NHS. Funding is approved on a case by case basis, with DSCs making individual funding applications to the VPP, which clearly set out the requirement and the benefit that is expected if the request is supported. More information is available on the NHS webpage on services for veterans with physical injuries.
Eligible veterans are also able to access the Complex Prosthetics Assessment Clinic (CPAC), which is run by Defence Medical Rehabilitation services. CPAC supports veterans with particularly complex prosthetic socket needs who have previously been seen at the Defence Medical Rehabilitation Centre Headley Court.
Veterans personalised care programme for ex-forces with a long term physical, mental or neurological health condition or disability
NHS England and NHS Improvement, together with the Ministry of Defence, have published the Personalised care for veterans in England, a guide for clinical commissioning groups and local authorities, which sets out a personalised care approach for those veterans who have a long term physical, mental or neurological health condition or disability.
This guide is for those individuals and organisations who are leading or involved in supporting this patient group through the delivery of NHS Continuing Health Care or a jointly agreed care plan. A supporting patient leaflet is also available.
Eligible individuals will have a single personalised care plan for all their health and wellbeing needs that is developed with them and a range of organisations, including health and social care and military charities. This approach will give the individual more choice and control over how their care is planned and delivered, meaning they can choose how best to live their life and get the right care and support to make this happen. It will also take into account personal preferences that relate specifically to the individual’s military service. As part of this, they may get a personal budget to pay for some of the care and support they need, as well as more support in the community, such as emotional and practical support from people who have similar health conditions or disabilities. To apply, individuals should contact their local clinical commissioning group.
The Veterans Covenant Health Alliance (VCHA)
The VCHA aims to improve NHS care for the Armed Forces community by supporting trusts, health boards and other providers to identify, develop and showcase the best standards of care. 33 hospital trusts have already been accredited as ‘Veteran Aware’, having demonstrated their commitment to eight core manifesto standards, including signing the Armed Forces Covenant, raising awareness of veterans’ healthcare needs among staff, and establishing links with local support providers. The VCHA is working with many more trusts to achieve accreditation.
More information on NHS services for veterans can be found on the NHS website here.
